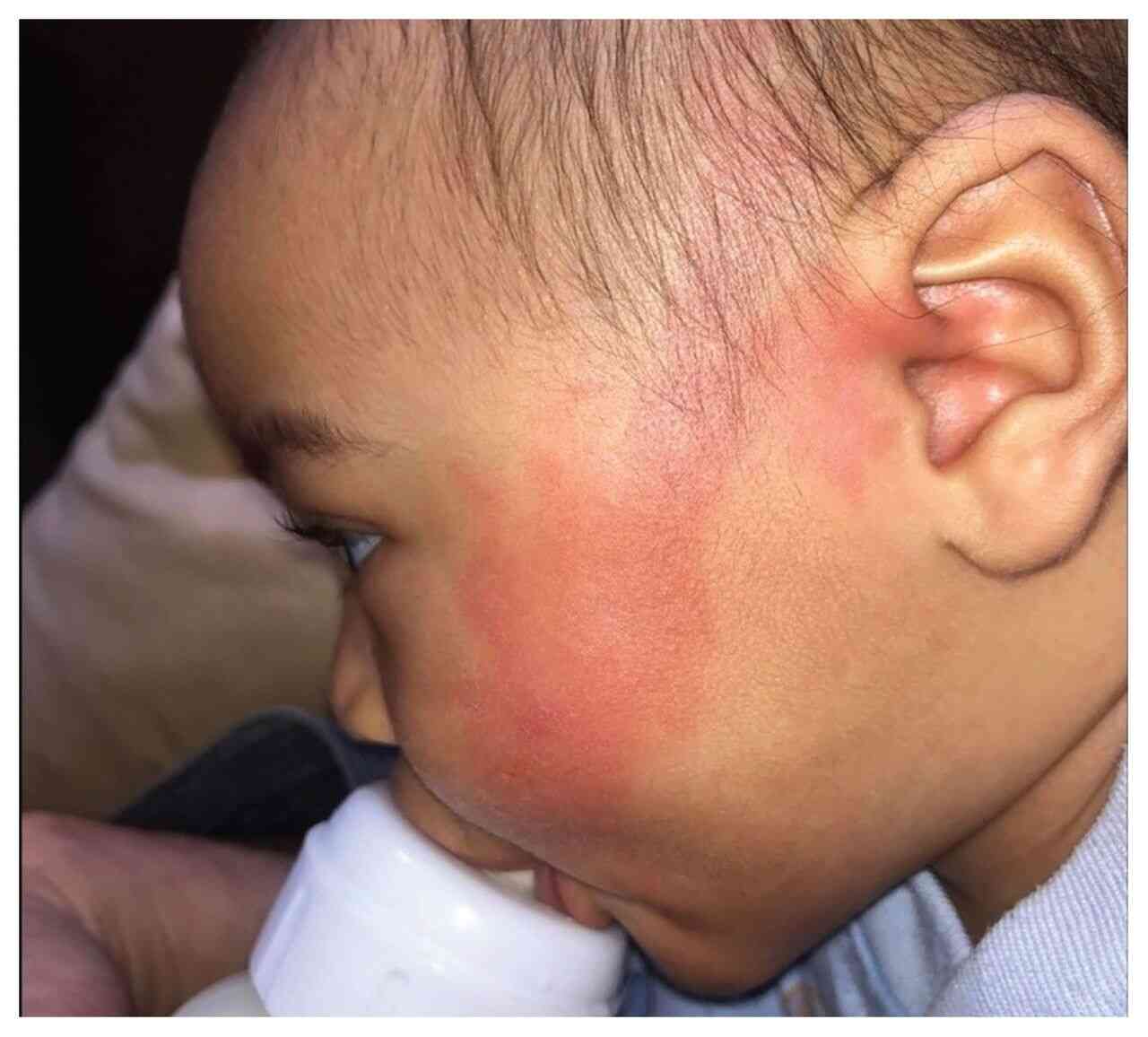
History: A healthy 1-year-old boy with the unremarkable medical history presented to a private clinic for a routine examination. Flushing & gustatory sweating was noted on the child’s left cheek. What’s the diagnosis?
Answer: Auriculotemporal nerve syndrome (Frey’s syndrome, Baillarger’s syndrome, Dupuy’s syndrome, or Frey-Baillarger syndrome) usually manifests as immediate unilateral or bilateral flushing, sweating in the distribution of the auriculotemporal nerve, or both in response to gustatory or tactile stimuli. In adults, this syndrome is a well-recognized sequela of parotid surgery, trauma, or infection. It occurs rarely in children, most often noted after the introduction of solid food. The flushing is often attributed erroneously to food allergy. It typically begins at 2–6 months of age when solid foods, mostly fruit, are introduced. Occurring within a few seconds of eating, it has a peculiar distribution in a triangular area that extends from the tragus of the ear to the midpoint of the cheek. It is not associated with sweating and persists for 20–60 min. The flushing continues to occur for up to 5 years. In adults, gustatory sweating is the predominant feature of auriculotemporal nerve syndrome; flushing happens less often. One-half of pediatric patients with this symptom were delivered with forceps assistance, which possibly causes trauma to the nerve. The likely mechanism is a misdirection of parasympathetic fibers along sympathetic pathways during the nerve regeneration that follows trauma. This may account for erythema when eating. The emergence of symptoms several months after the proposed trauma (usually 3–6 months) is probably related to the time required for nerve regeneration, and it is possible that vigorous chewing causes intense stimulation of the parotid gland.