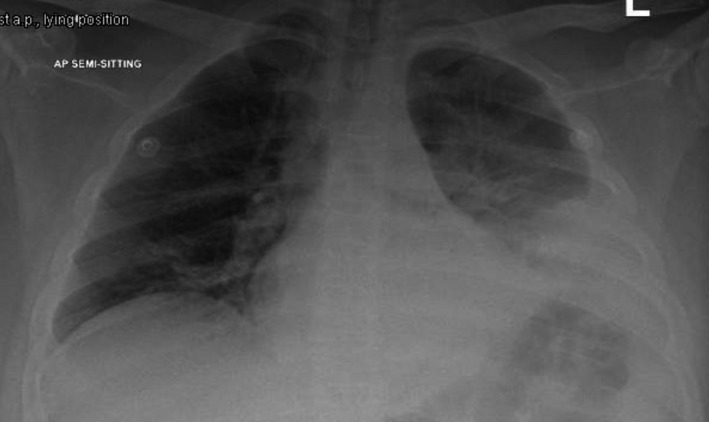
History: A 16-year-old male patient who is known to have HBSS disease, presented with a history of chest and back pain for a few days prior to admission. He also complained of a nonproductive cough for 2 days but denied fever. On examination, his HR 110, RR 25, Temp – 103F. On chest exam, he had left basal crackles with decreased air entry. His chest x-ray showed left retrocardiac and left lower lung zone opacity suggesting left lower lobe consolidation. What is the likely diagnosis?
Answer: Acute chest syndrome is a vaso-occlusive crisis of the pulmonary vasculature commonly seen in people with sickle cell anemia. This condition commonly manifests with a new opacification of the lung(s) on a chest x-ray.
Signs and symptoms:
ACS is defined by a new pulmonary density on chest imaging involving at least one complete lung segment and at least one of the following [68]:
- Temperature ≥38.5°C
- >3 percent decrease in SpO2 (oxygen saturation) from a documented steady-state value on room air
- Tachypnea (per age-adjusted normal)
- Intercostal retractions, nasal flaring, or use of accessory muscles
- Chest pain
- Cough
- Wheezing
- Rales
Investigations: CBC, CXR, Blood culture, LFT, KFT, ABG
Treatment: Bronchodilators, Antibiotics, Supplemental oxygen, Non-invasive/ invasive ventilation.