History: A 60 year old woman nursing home patient with Type2DM, HTN, and a prior haemorrhagic stroke presented to ED with progressive dyspnoea, cough with white sputum and low-grade temperature. On arrival, the patient was tachypnoeic, using accessory muscles and oxygen desaturation was noted. Physical examination showed no jugular vein engorgement, trachea was not deviated and auscultations revealed bilateral equal breath sounds with bi-basilar rales. Despite supplemental oxygen, the patient required intubation and was admitted to ICU. However, in the ICU, the patient’s saturation continued to fluctuate despite varying ventilation settings. What is the most likely cause of respiratory failure in the patient?
-
Pulmonary oedema
-
Pneumonia
-
Pneumothorax
-
Foreign body aspiration
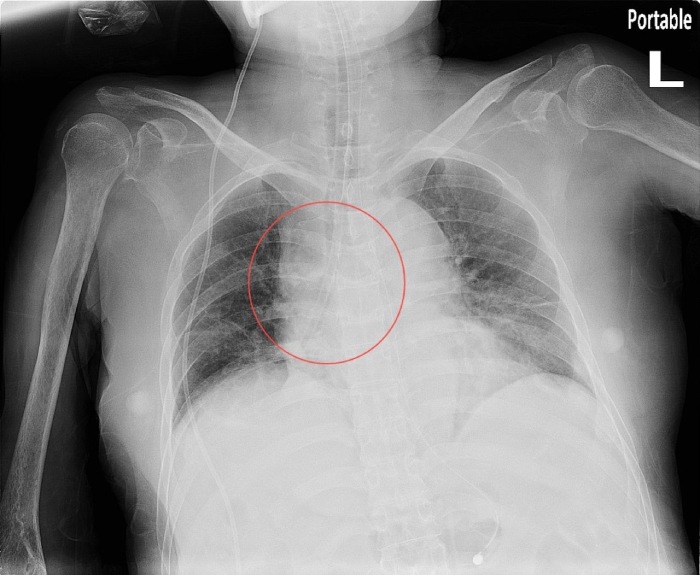
Answer: The foreign body in the right bronchus. The foreign body was later found to be a suction tube used by the nursing home, which was suspected to have broken off at some point for unknown reason.
The ABCDEFGHI mnemonic is very useful: A stands for assessment of quality and airway. The X-ray here was a supine AP view, with poor inspiration of only six posterior rib visible, and reviewing the airway, there was no tracheal deviation, the endotracheal tube was in place but a suspicious object could be seen in the right bronchus. The rest of the mnemonic would be: B for bones and soft tissue (no bone fractures and no subcutaneous air). C for cardiac silhouette, D for diaphragm, E for effusion, F for fields, fissure and foreign body, (pneumonia, pulmonary oedema and pneumothorax) are not seen but there are three foreign bodies: the endotracheal tube, VP shunt and again, one in the right bronchus, G for gastric bubble and great vessels, H for hila and mediastinum and lastly I for impression. Using this standardised approach, we would have a greater chance of identifying the foreign body and thus provide more timely management for the patient.