History: A 45-year-old male is brought to the Emergency Department after a high-speed road traffic accident. He was the unrestrained driver, found unconscious at the scene.
Prehospital: EMS reports shallow breathing, SpO₂ 80% on room air. No IV access secured. Cervical collar applied at the scene.
On Arrival (Primary survey):
-
- General appearance: Unresponsive, pale, cold extremities.
- Airway: Gurgling sounds, blood in oral cavity.
- Breathing: RR 8/min, SpO₂ 82% RA, bilateral decreased breath sounds.
- Circulation: Pulse 130/min, BP 80/50 mmHg, cap refill >3 sec.
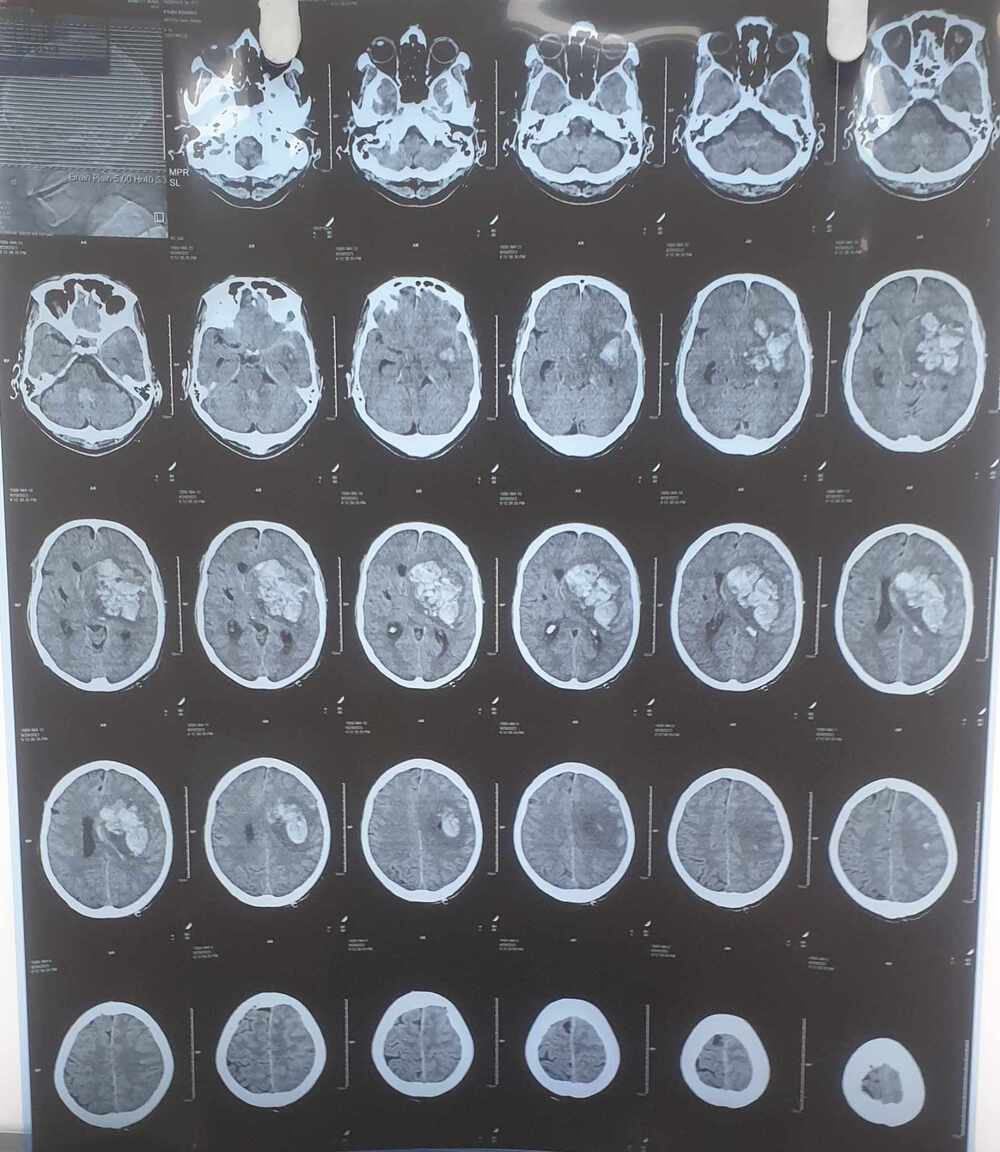
- Disability: GCS 7/15 (E2V2M3), pupils equal and reactive.
- Exposure: Multiple abrasions, right thigh deformity, abdominal distension
How to Approach This Patient in ED
Step 1: Primary Survey – ABCDE
A – Airway with Cervical Spine Protection
- Airway suctioned, jaw thrust performed.
- Oropharyngeal airway inserted → proceeded with Rapid Sequence Intubation (RSI).
- Cervical spine maintained with collar and inline stabilization.
👉 Rationale: GCS <8 indicates inability to protect airway. In trauma, always assume cervical spine injury until ruled out.
B – Breathing
- Bag-valve-mask ventilation with 100% O₂ until intubation completed.
- Bilateral auscultation confirmed equal air entry post-intubation.
- Continuous pulse oximetry and ETCO₂ monitoring.
👉 Rationale: Hypoventilation and hypoxemia corrected; must always rule out tension pneumothorax/hemothorax.
C – Circulation with Hemorrhage Control
- 2 large-bore IVs secured; blood drawn for CBC, type & crossmatch, coagulation profile, ABG, lactate.
- IV fluids: 1L warm crystalloids (permissive hypotension until hemorrhage controlled).
- Massive transfusion protocol (MTP) activated (PRBC:FFP:Platelet = 1:1:1).
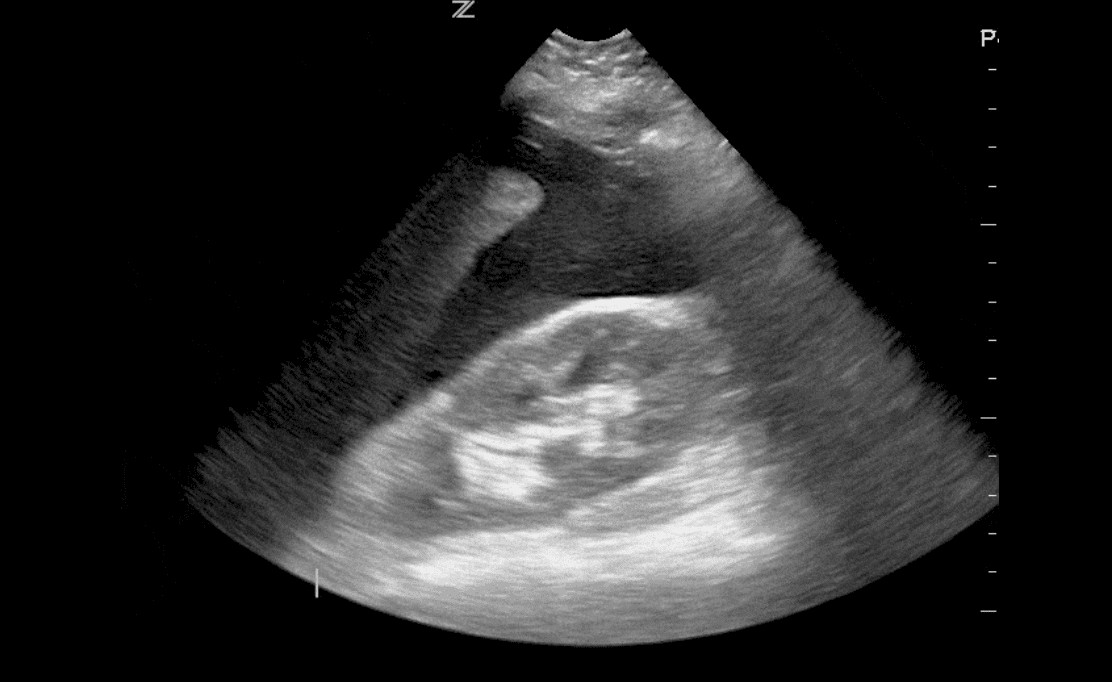
- FAST scan positive for intra-abdominal free fluid → urgent surgical consult.
👉 Rationale: Patient in hemorrhagic shock; early balanced transfusion is lifesaving.
D – Disability (Neurological)
- GCS reassessed post-intubation.
- Blood glucose checked (normal).
- Neurosurgery consult due to severe TBI.
👉 Rationale: GCS <8 → severe head injury. Always check glucose as reversible cause.
E – Exposure & Environment
- Patient fully undressed; pelvic binder applied for suspected pelvic fracture.
- Femur stabilized with traction splint.
- Warm blankets used to prevent hypothermia.
👉 Rationale: Trauma requires full exposure to identify hidden injuries, but hypothermia worsens coagulopathy.
Step 2: Adjuncts & Secondary Survey
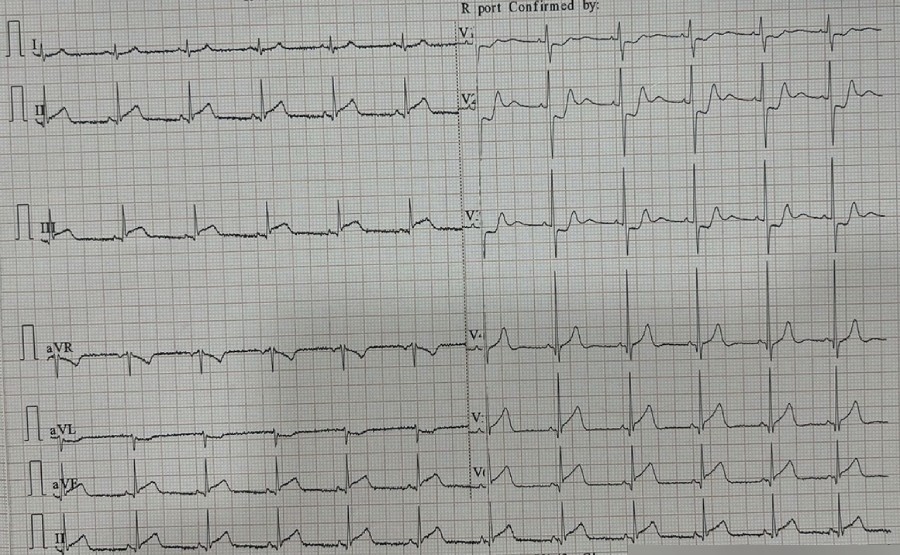
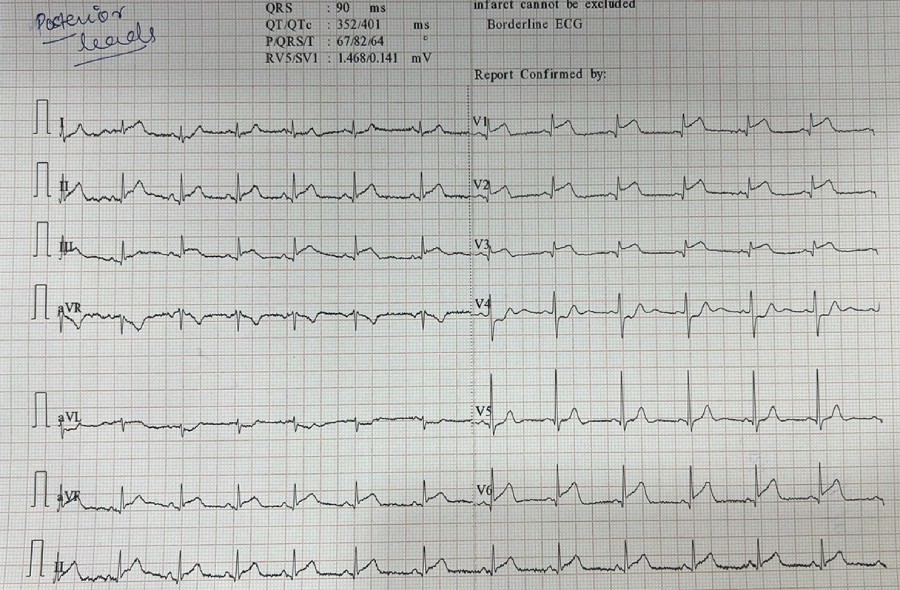
- Monitoring: ECG, SpO₂, ETCO₂, NIBP/arterial line.
- Investigations: ABG, chest X-ray, pelvis X-ray, CT head/abdomen (when stable).
- Secondary survey: Detailed head-to-toe exam, history from EMS/family.
- Definitive care: Patient requires exploratory laparotomy for intra-abdominal bleeding.
Key teaching points for residents:
- Airway management is first priority – GCS <8 mandates intubation.
- Cervical spine protection is non-negotiable in trauma.
- Shock in trauma is hemorrhagic until proven otherwise.
- Use damage control resuscitation – permissive hypotension, massive transfusion, avoid excess crystalloids.
- FAST scan is the quickest bedside tool for intra-abdominal bleeding.
- Hypothermia prevention is critical (part of trauma “lethal triad”).
- Early multidisciplinary involvement (surgery, neurosurgery, orthopedics).





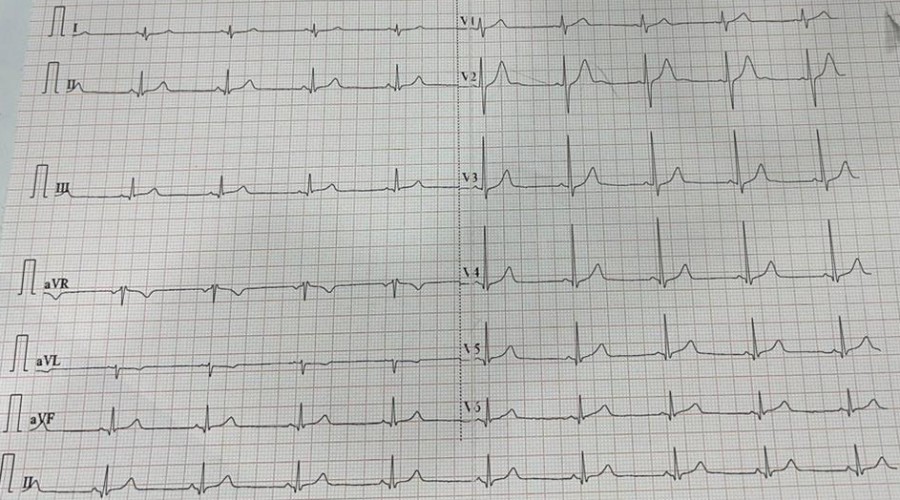
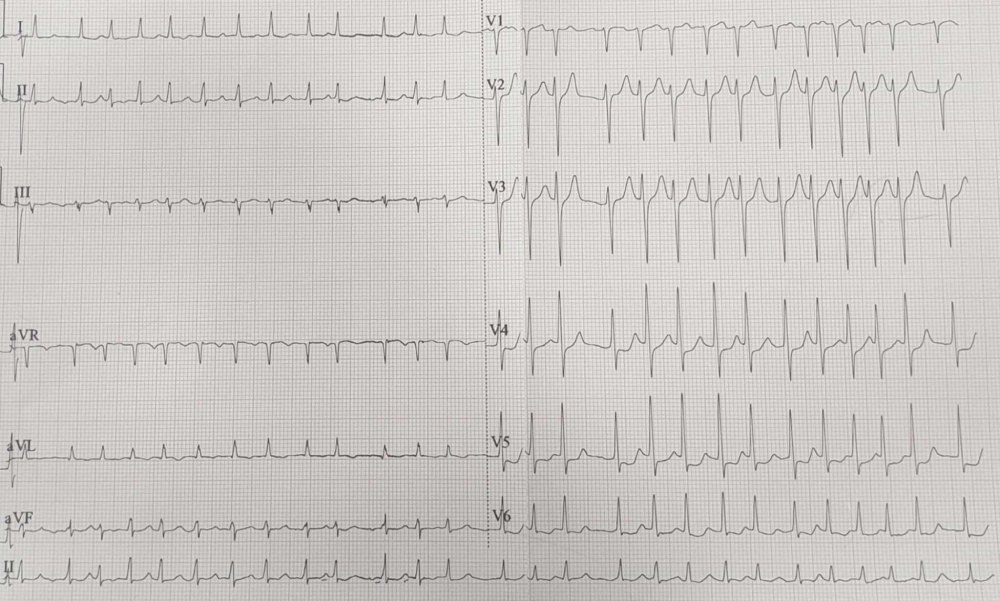



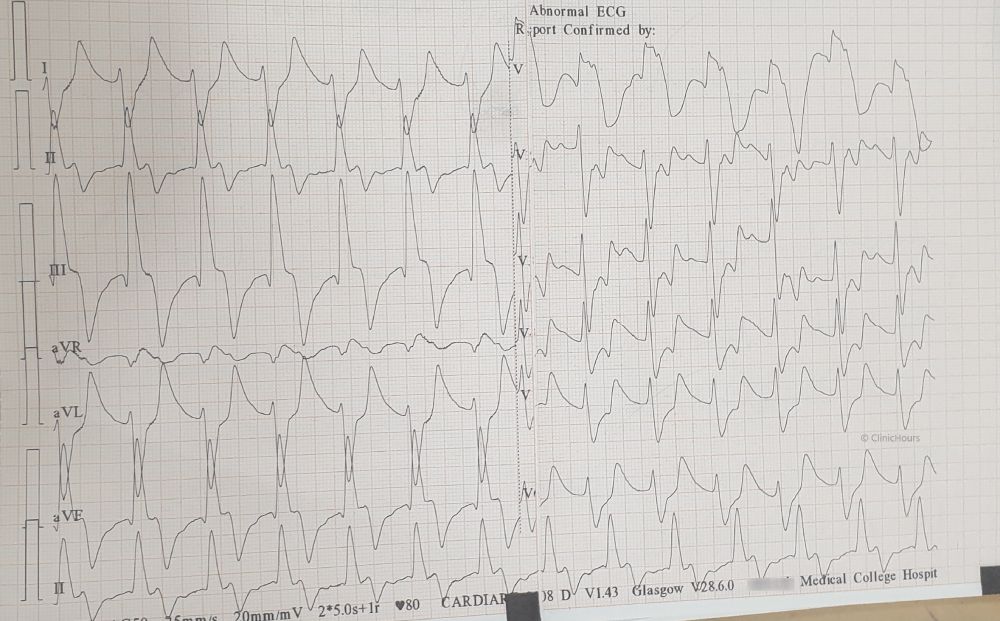
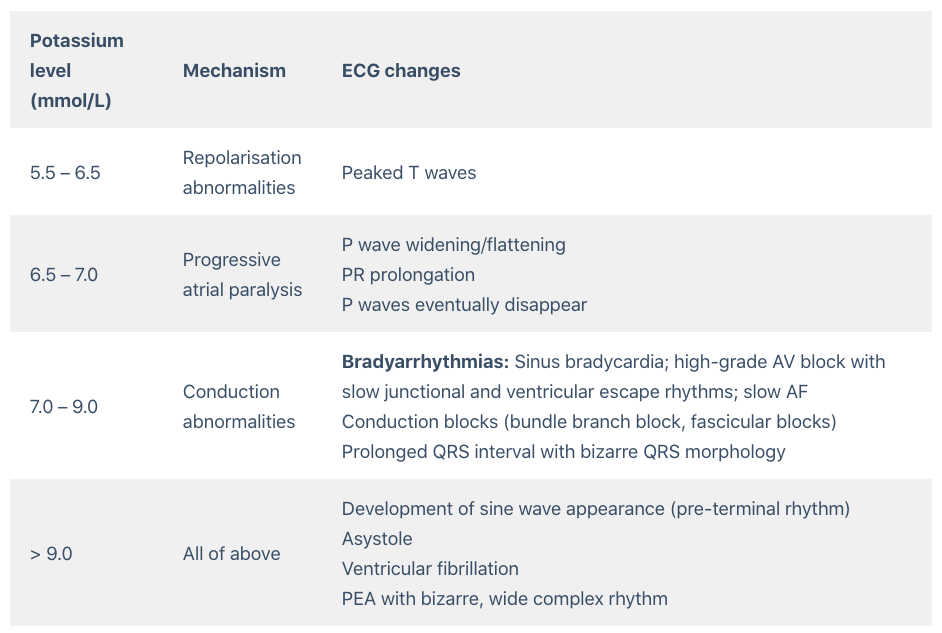 The patient was treated with 10% 10ml of IV calcium gluconate, nebulised with Salbutamol, 10 units of regular insulin IV combined with dextrose 50%, IV sodium bicarbonate 50 mEq and Inj. Furosemide 40mg IV. Emergent haemodialysis was initiated. Pt was shifted to ICU.
The patient was treated with 10% 10ml of IV calcium gluconate, nebulised with Salbutamol, 10 units of regular insulin IV combined with dextrose 50%, IV sodium bicarbonate 50 mEq and Inj. Furosemide 40mg IV. Emergent haemodialysis was initiated. Pt was shifted to ICU.