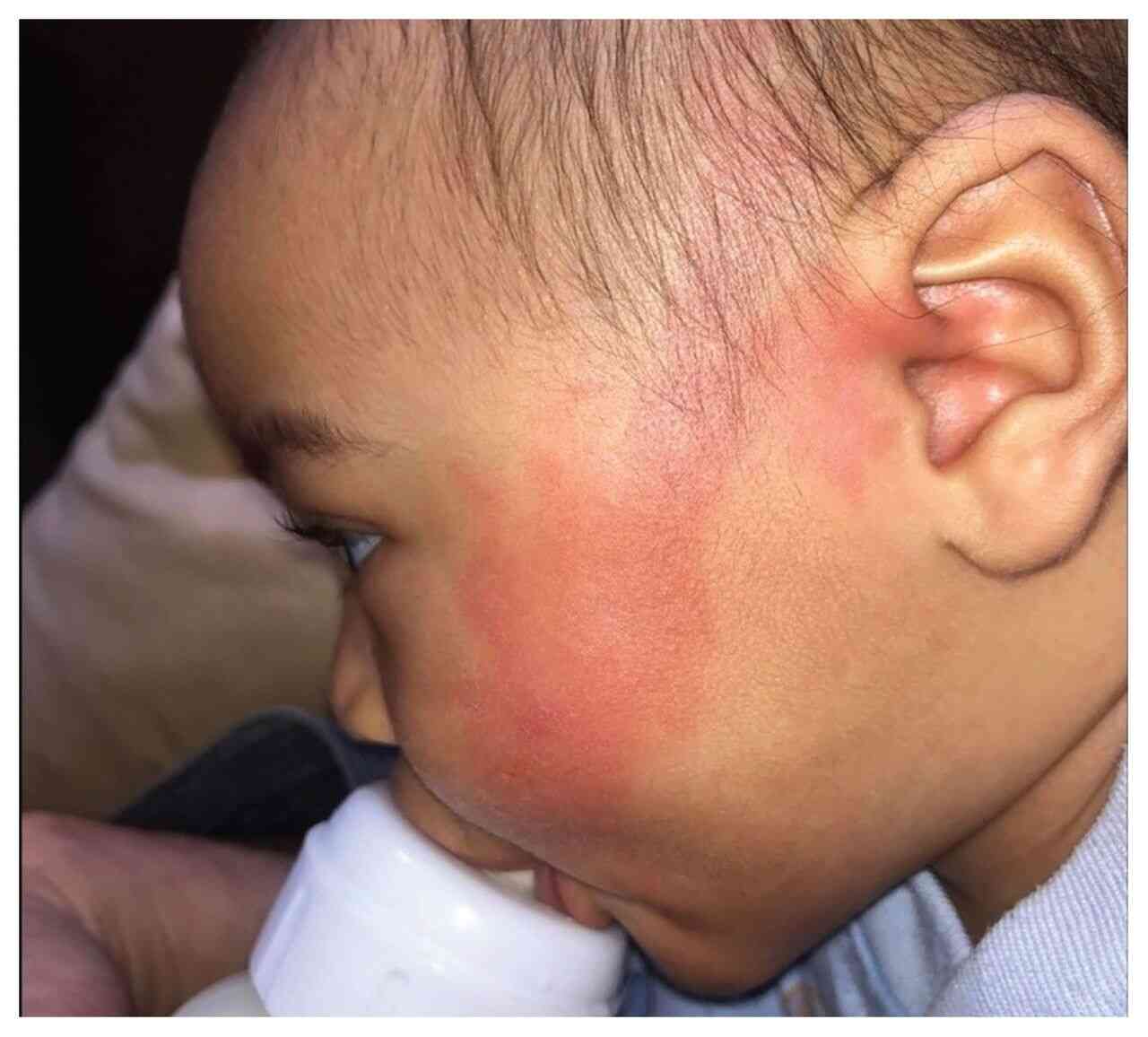
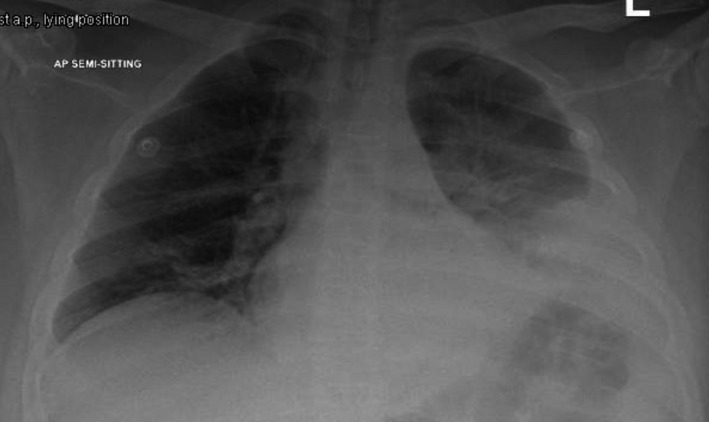
History: A 60 yr old male had developed livedo reticularis on the left side of his face after he underwent stenting and balloon dilation of the left common carotid artery. Shivering, sweating, and confusion developed immediately after artery dilation, along with a left gaze preference, dysarthria, and hemiparesis on the right side of his body. Angiography showed a patent left internal carotid artery and an occluded distal left facial artery. No IC bleed on NCCT head. What’s the diagnosis?
Answer: The patient was transferred to the ICU, where MRI angiography of the brain revealed infarctions in the territory of the left middle cerebral artery with patent vasculature. An acute embolic stroke and cholesterol embolization syndrome of the face was diagnosed. In cholesterol embolization syndrome, atherosclerotic plaque contents from large-caliber arteries embolize to smaller arteries and lead to vascular occlusion, inflammation, and end-organ damage. Livedo reticularis is one of the most common skin manifestations of the syndrome. The patient received supportive care in the ICU. The livedo reticularis resolved 1 week after the event, but the neurologic deficits persisted at the time of his discharge from the hospital.