The 2023 GOLD report contains numerous updates:
Chapter 1
► A new definition of COPD has been proposed (Page 5)
► A section on Chronic Bronchitis has been added (Page 13)
► A table has been added with Proposed Taxonomy (Etiotypes) for COPD (Table 1.1)
Chapter 2
► Additional information on screening for COPD and case-finding has been included (Page 36)
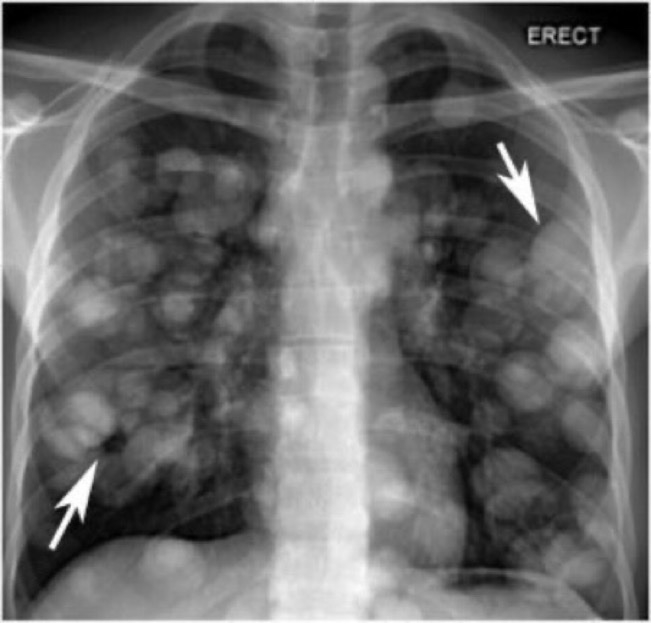
► Information on Imaging and Computed Tomography (CT) has been included (Page 43)
► A table with information on the Use of CT in Stable COPD has been added (Table 2.8)
Chapter 3
► Vaccination Recommendations for people with COPD have been updated in line with current guidance from the CDC (Page 54)
► Further information on therapeutic interventions to reduce COPD mortality has been added (Page 67)
► A table has been added with information on the Evidence Supporting a Reduction in Mortality with Pharmacotherapy and Non-pharmacotherapy in COPD Patients (Table 3.6)
► Issues Related to Inhaled Delivery have been addressed (Page 69)
► Information on the topic of Adherence to Inhaled COPD Medications has been included (Page 71)
► A section on Tele-rehabilitation has been added (Page 76) Page 2 of 16
► The section on Interventional & Surgical Therapies for COPD has been expanded (Page 82)
► A figure has been added giving an Overview of Current and Proposed Surgical and Bronchoscopic Interventions for People with COPD (Figure 3.2)
Chapter 4
► A section on the choice of inhaler device has been added (Page 112)
► A table has been added with information on Basic Principles for Appropriate Inhalation Device Choice (Table 4.5)
► The ABCD Assessment Tool has been revised to the ABE Assessment Tool to recognize the clinical relevance of exacerbations, independent of the level of symptoms (Page 115)
► The information and figures outlining Initial Pharmacological Treatment and Follow-up Pharmacological Treatment have been updated. In particular, the positioning of LABA+LAMA and of LABA+ICS has been changed (Page 115)
Chapter 5
► The topic of management of exacerbations has been expanded to include details of possible alternative causes
of symptoms
► A new definition of COPD Exacerbation and a new set of parameters to assess exacerbation severity at the point of care has been included (Page 134)
► A new paragraph and a new figure on the Classification of the Severity of COPD Exacerbations have been added (Figure 5.1)
► A new table on Diagnosis and Assessment has been added (Table 5.3)
Chapter 6
► The chapter on COPD and Co-morbidities has been updated with the latest evidence.
Chapter 7
► The chapter on COVID-19 and COPD has been updated with new references and the latest evidence.
Download 2023 GOLD guide